Everything You Should Know About Erectile Dysfunction

Erectile dysfunction—often shortened to E.D.—is one of those things almost every man will experience at some point in his life, yet few ever talk about. It can feel confusing, frustrating, or even shameful when your body doesn’t respond the way you expect it to. But here’s the truth: you’re not broken, you’re not alone, and it’s more common than you think.
E.D. can show up for a lot of reasons—some physical, some mental, some just part of everyday life. Understanding where it’s coming from is the first step toward taking back control of your sexual confidence.
The Three Faces of Erectile Dysfunction
Physical/Medical Reasons:
Sometimes, E.D. has a straightforward medical root. Conditions like diabetes, heart disease, nerve damage, or even certain medications can interfere with the complex blood flow process that causes an erection.
The good news? When the underlying issue is treated, erectile function often improves.
Mental Health Reasons:
Other times, the mind plays a starring role. Stress, anxiety, depression, or substance use can all impact sexual response.
In fact, performance anxiety—that spiral of “What if it doesn’t happen again?”—is one of the most common psychological triggers.
And because mental and physical factors often overlap, you might find that addressing one helps the other.
Everyday, Temporary Reasons:
Then there are the short-term culprits: a long week, too many drinks, not enough sleep, or everyday stress. These moments don’t necessarily point to a deeper problem. They happen, they pass, and they don’t define you.
How Common Is E.D.?
According to the National Kidney and Urological Disease Center, physician visits for erectile dysfunction nearly tripled between 1985 and 1999—thanks in part to the growing acceptance of talking about it and the rise of treatments like Viagra® and vacuum devices.
“The incidence increases from about 5% of men at age 40 to between 15–25% of men at age 65.” That’s millions of men, across every background and body type, dealing with the same thing you are.
So if you’re experiencing it, take a breath—you’re in very good company.
How Erections Actually Work
Think of an erection as a finely tuned symphony between your brain, nerves, blood vessels, and hormones — all playing in perfect rhythm. When even one instrument is off, the entire performance can falter.
Let’s break down what’s really going on beneath the surface.
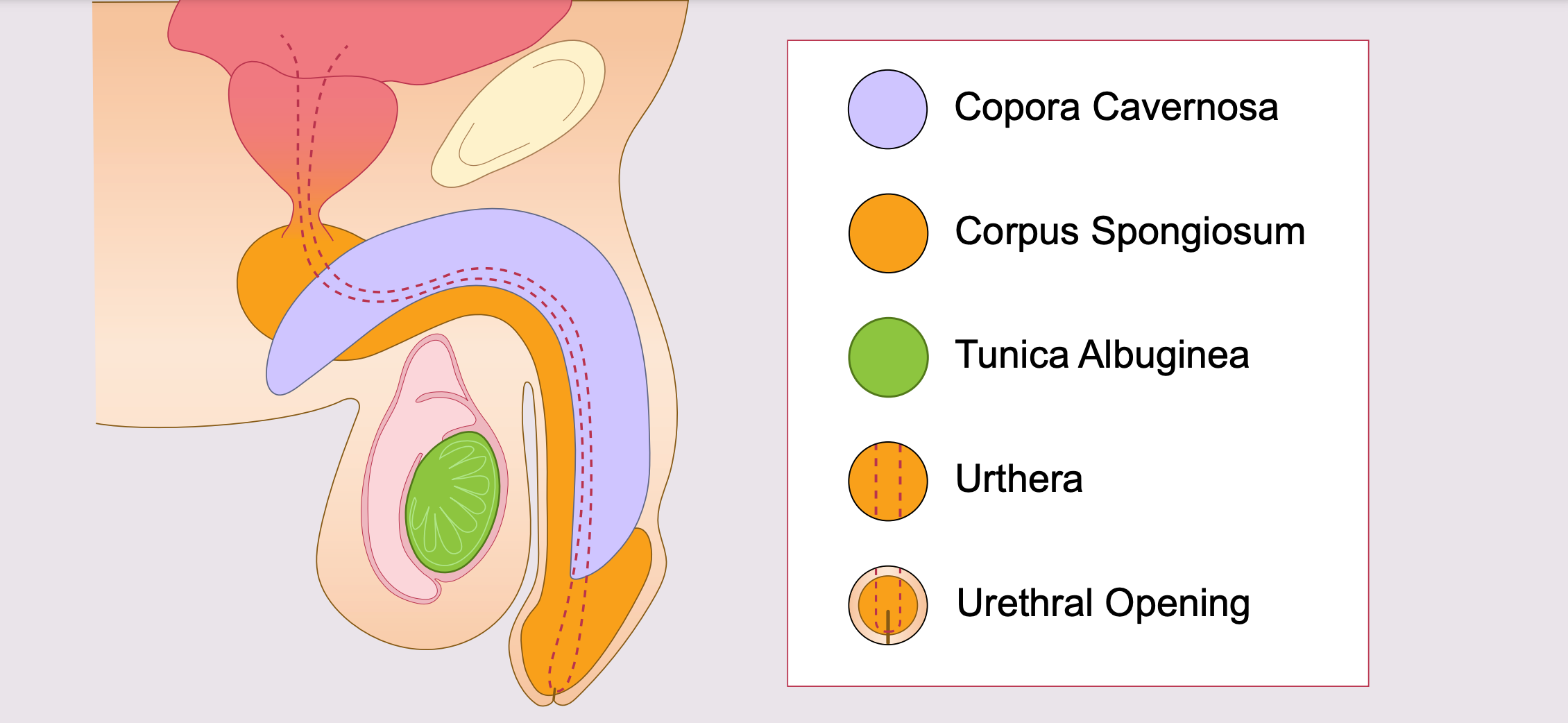
The penis is made up of three main columns of erectile tissue:
-
Two corpora cavernosa – These run along the top of the penis and are primarily responsible for creating firmness.
-
One corpus spongiosum – This runs along the underside and surrounds the urethra, the channel that carries both urine and semen to the urethral opening at the tip.
All three columns are wrapped in a tough, fibrous sheath called the tunica albuginea, which acts like the outer wall of a balloon — it stretches to accommodate incoming blood but also traps it in place to maintain rigidity.
Inside these chambers is spongy tissue made of smooth muscle, fibrous tissue, veins, and arteries — the plumbing and structure that make erections possible.

Can It All Be In My Head?
Psychological factors can be powerful. Around 10–20% of E.D. cases stem from mental or emotional causes like stress, trauma, relationship strain, or self-esteem issues. (National Kidney and Urological Disease Center, 2017).
The mind is a powerful tool - and while it helps to get you aroused (through visual stimulation, internal narratives and thought processes) it can also be the downfall of your erection.
Performance anxiety is one of the biggest culprits. It often starts with a single difficult experience—maybe you were tired, anxious, or distracted—and suddenly your body didn’t respond the way you expected. The next time, you start to worry it might happen again. That worry activates your body’s stress response, which tightens blood vessels and floods you with cortisol, making it even harder to get or stay hard. The cycle repeats, feeding itself with each new anxious thought.
Many men notice they can achieve and maintain erections easily during masturbation, but not during partnered sex—and that’s completely normal. Solo play feels safe and pressure-free, while intimacy can bring vulnerability, expectations, and sometimes the fear of “failing.” Over time, that stress can lead to avoidance, frustration, or even feelings of shame.
The best antidote? Communication and compassion—both for yourself and your partner. Talk openly about what’s happening instead of bottling it up. Most partners are far more understanding than you might expect. And remember: intimacy isn’t defined by penetration. It’s about closeness, connection, and pleasure in all its forms—touch, laughter, eye contact, and emotional safety all count.
When you shift the goal from “performance” to shared enjoyment, your body often follows suit naturally. Sometimes, taking the pressure off is the first step toward getting your confidence—and your erections—back.
If anxiety, depression, or past experiences are making this cycle hard to break, a licensed therapist or certified sex therapist can help you untangle the emotional roots of E.D. You don’t have to navigate it alone—professional support can be one of the most effective (and liberating) tools for getting back in touch with your body.
Shop Our Full Collection of Hollow Strap-Ons - Click Here!
How Stress & Lifestyle Play a Role
Modern life isn’t exactly calm. Work, finances, aging, health—all of it takes a toll. Chronic stress triggers hormones that constrict blood vessels and dampen arousal.
Gentle movement like yoga, stretching, or regular exercise can improve circulation and reduce anxiety. Managing your stress doesn’t just help your sex life—it improves your overall well-being.
Getting the Help You Need
If E.D. has become more than a once-in-a-while occurrence, it’s time to check in with a professional. Think of it as gathering data—not admitting defeat.
Step 1: Talk to Your Doctor
Your primary care provider has heard it all before. Truly—this is one of the most common topics men bring up, even if it doesn’t always feel that way. A simple conversation can help determine whether your E.D. stems from physical factors (like blood flow or hormones), psychological factors (like anxiety or stress), or a mix of both.
Be open about what’s happening, including when and how often it occurs, whether it’s different during solo play, and any medications or lifestyle factors that might play a role. The more detail you share, the faster you can find real answers.
Step 2: Testing
Your doctor may order a few straightforward tests—typically bloodwork to check testosterone, blood sugar, cholesterol, and circulation markers. These can reveal whether issues like low testosterone, diabetes, or heart disease are contributing factors.
If something’s off, small adjustments can make a big difference: improving your diet, adding light exercise, cutting back on alcohol, or managing blood pressure can all boost erectile health. In some cases, your doctor might also review medications that could be interfering with arousal or blood flow.
Step 3: Urology Consultation
If your initial tests look normal but symptoms persist, your doctor may refer you to a urologist—a specialist in male sexual and urinary health. A urologist can perform more targeted exams such as a penile Doppler ultrasound, which measures blood flow and vascular function, or nerve tests to rule out neuropathy. These assessments help pinpoint what’s happening inside your body with precision.
Step 4: Consider Mental Health Support
If your doctor suspects stress, anxiety, or other emotional factors, seeing a therapist or certified sex therapist can be transformative. Therapy can help break the mental loop that turns one difficult experience into recurring anxiety, and teach you techniques to rebuild confidence and rekindle pleasure.
In many cases, a combined approach works best—addressing both the physical and psychological sides of E.D. helps men recover faster and maintain results longer.
Treatment Options That Can Help
Depending on what you and your clinician uncover, there are several paths—some well-established, others emerging.
Tried-and-True Options
-
Oral medications (PDE-5 inhibitors): Sildenafil (Viagra®), Tadalafil (Cialis®), Vardenafil (Levitra®, Staxyn®), and Avanafil (Stendra®) improve penile blood flow and are first-line for many men. They differ in onset, duration, and side-effect profiles—your provider can help you match the med to your needs.
-
Lifestyle shifts: Consistent exercise, weight management, quitting smoking, moderating alcohol, and better sleep all support vascular health (and erections).
-
Devices: Vacuum erection devices (penis pumps) can create a firm erection on demand; a constriction ring may help maintain it after pumping.
-
Therapy & sex therapy: If anxiety, stress, or relationship dynamics are involved, working with a therapist (especially a sex therapist) can be game-changing—on its own or alongside medical treatment.
-
Other medical options: Depending on the cause, clinicians may consider testosterone optimization (when clearly deficient), intracavernosal injections, intraurethral meds, or in select cases surgery/implants.
What’s New or On the Horizon
These options are investigational or not universally recommended yet. Discuss risks/benefits with a qualified clinician.
-
Melanocortin activators (e.g., PT-141):
Act centrally (in the brain) rather than on blood vessels. Early human studies—especially intranasal forms—suggest potential benefit for psychogenic or mild–moderate E.D. Larger trials are needed to confirm safety and effectiveness. -
Low-intensity shockwave therapy (Li-SWT):
A non-invasive approach under study that uses gentle acoustic waves to stimulate new blood vessel growth and improve penile blood flow. Promising for vascular E.D., but protocols vary and regulatory guidance is evolving. -
Gene therapy:
Experimental strategies aim to deliver genes that restore or enhance proteins involved in erection within penile tissue. Animal data are encouraging; human use will require more research and regulatory approval. -
Stem cell therapy:
Uses autologous or donor stem cells to repair endothelial/penile tissue. Results are inconsistent and can depend on the cell source and protocol. Still investigational. -
Platelet-rich plasma (PRP):
Although platelets support healing, current studies show little to no benefit for E.D. at this time.
A gentle reminder
-
Even with exciting research, PDE-5 inhibitors, lifestyle optimization, counseling, and evidence-based devices remain the backbone for most men.
-
Before trying anything new (especially “regenerative” clinics or cash-based treatments), talk to your healthcare provider about quality evidence, realistic outcomes, cost, and safety.
Your path doesn’t have to be perfect to be effective. With the right mix of medical guidance, patience, and pressure-free intimacy, it’s absolutely possible to feel confident and connected again.
Reconnecting Intimately
E.D. doesn’t have to mean the end of pleasure. In fact, many couples say that navigating it strengthened their connection.
Explore pleasure in new ways:
-
Oral sex, mutual masturbation, and sensual touch can all create closeness and satisfaction.
-
Try “no-pressure nights” where sex isn’t the goal—just connection.
-
Experiment with toys designed for mutual pleasure. A simple couple’s vibrator or male stroker can reignite excitement while easing anxiety.
Some couples even explore Tantric sex, which emphasizes breath, energy, and intimacy over performance. Remember, pleasure is about connection—not perfection.
Therapy & Emotional Healing
For those whose E.D. has roots in anxiety or self-doubt, sex therapy can be transformative. Techniques like sensate focus therapy teach couples how to rebuild touch and trust slowly, without pressure to “perform.”
As one therapist puts it, “We’re not trying to fix your erection—we’re rebuilding your comfort with pleasure.”
Final Thoughts: Be Kind to Yourself
Erectile dysfunction can shake your confidence—but it doesn’t define your masculinity or your worth. It’s simply a sign that something (physical, emotional, or both) needs care.
If you take anything from this, let it be this:
-
You’re not alone.
-
You’re not broken.
-
And there are effective, compassionate ways forward.
With the right mix of medical support, patience, and open communication, you can absolutely regain your confidence, your connection, and your pleasure.
Your sex life isn’t over—it’s just entering a new chapter.
References
Health University of Utah. “Shock Wave Therapy for Erectile Dysfunction.” University of Utah Health, 2023. https://healthcare.utah.edu/healthfeed/postings/2023/02/shock-wave-therapy-ed.php
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Definition & Facts for Erectile Dysfunction (ED).” Updated October 2024. U.S. Department of Health and Human Services. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/definition-facts
National Kidney and Urological Disease Information Clearinghouse. “Erectile Dysfunction.” National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), 2017. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction
Sexual Health & Healing LLC. “What Is Sensate Focus Therapy.” SexualHealthAndHealing.org. Accessed 2025. https://sexualhealthandhealing.org/what-is-sensate-focus-therapy/
University of Utah Health. “Shockwave Therapy for Erectile Dysfunction (ED).” HealthCare University of Utah, February 19 2025. https://healthcare.utah.edu/mens-health/conditions/erectile-dysfunction/shockwave-therapy
WebMD Editorial Contributors. “Future Treatments for Erectile Dysfunction.” WebMD, last reviewed July 13, 2025. Medically reviewed by Nazia Q. Bandukwala, DO. https://www.webmd.com/erectile-dysfunction/future-treatments
Books you may find helpful:
- Coping With Erectile Dysfunction: How to Regain Confidence and Enjoy Great Sex by Michael E., Ph.D. Metz and Barry W., Ph.D. McCarthy
- An Atlas of Erectile Dysfunction by Roger S. Kirby
- Rekindling Desire: A Step-by-Step Program to Help Low-Sex and No-Sex Marriages by Barry W. McCarthy and Emily J. McCarthy
4 comments
![["<div", "class=\"metafield-rich_text_field\"><p><strong>Article", "Reviewed", "and"]](http://www.tootimid.com/cdn/shop/files/dr-image-001.png?crop=center&height=75&v=1712236737&width=75)








![["<div", "class=\"metafield-rich_text_field\"><p><strong>Article", "Reviewed", "and"]](http://www.tootimid.com/cdn/shop/files/dr-image-001.png?crop=center&height=50&v=1712236737&width=50)


I’m tryina earn somethin… On the cool
I’m a Veteran that was exposed to Agent Orange. Which caused me to be a Type 2 Diabetic, and another side effect of Agent Orange is ED, and Heart Issues. I’m 75 yrs of age and I haven’t had an erection for several years, however I can still achieve an orgasm & my wife and I explored together options thar have helped both of us.
I strongly recommend Too Timid, the people & products have been very helpful
Thank you for sharing that article. Very informative. I’ve been on V.A healthcare since the year 2000 and have always had top notch treatment. In 2010 one of my doctors started me on prostate meds, those were Tamsilosun and finesteride. Now me being a firm believer in Drs. doing right by you, I just took them everyday like the lable said. Well, 7 or 8 years down the road it seems somethings not right. A good friend brought to my attention the side effects section of pharmacy literature for both those drugs. They both mention “Decreased sexual ability”., which means your sex life is over. Do the math, everyday for 14 years, that might be Algebra.
Leslie I guess I’ll go shopping while I’m here.
Thanks for the info. One of the many reasons I shop your company.
Leave a comment